
From the lab of Cheng Zhu: Integrin, vital proteins that play a major role in hemostasis and thrombosis, biomechanically facilitate platelet aggregation
When you nick yourself shaving, or clumsily slice your thumb while cutting sheetrock, you can thank goodness for integrins. These specialized proteins play a critical role in stopping the bleeding that ensues as a result of the aforementioned maladies (and other such breaches of the skin).
“Integrins are cell membrane receptors that mediate cell adhesion and mechanosensing,” explains Cheng Zhu, Regents Professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University.
They are vital to cellular biological processes, such as growth and development – cell attachment to the extracellular matrix (ECM) is a basic requirement in building a multicellular organism, for instance.
Following the mishaps described above, your platelets (which utilize the binding and signaling functions of an integrin called glycoprotein IIb/IIIa, or αIIbβ3) swarm the wound and clump together, forming a plug, or clot to stop blood loss. This first stage of wound healing is called hemostasis.
“Of course, the other side of the coin is thrombosis, which is what kills people who have cardiovascular disease,” says Zhu, a researcher in the Petit Institute for Bioengineering and Bioscience at Georgia Tech, describing what happens when platelet clumping runs amok, causing deadly clots.
So integrins basically facilitate how cells bind to and respond to their environment. They allow cells to cling to the ECM and to each other, and they are great communicators, transmitting bi-directional signals: inside-out, to activate the binding function; and outside-in, allowing the cell to sense and react to the extracellular environment. The integrin can instruct the cell.
But the mechanisms behind these important processes remain poorly understood, which is why Zhu and an international team of researchers are digging into integrins.
“This is a very important, dynamic biological molecule, a little nanomachine with hinges and moving parts,” says Zhu, co-corresponding author of a research paper in the journal Nature Materials, entitled, “When this integrin takes an intermediate structure, it has an intermediate affinity, and this intermediate state mediates biomechanical platelet aggregation.”
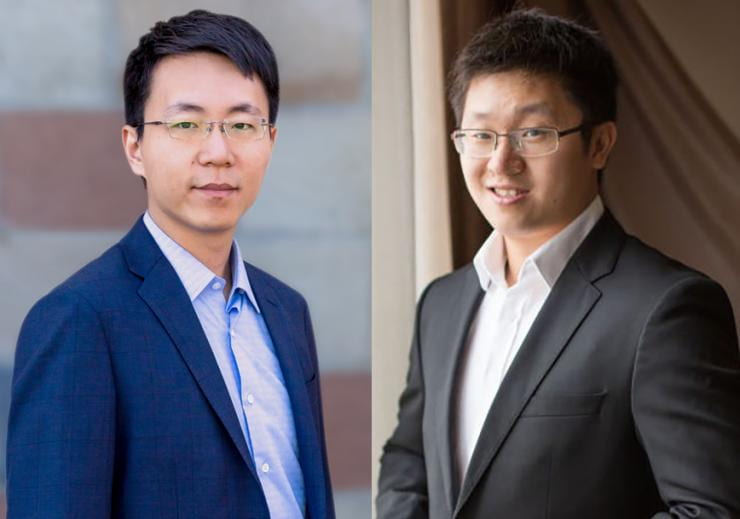
This is actually a continuation of research that began several years ago by former grad students in Zhu’s lab, where a major focus is on the biomechanics and mechanobiology of cell adhesion and signaling molecules of the immune system and vascular systems. The former Georgia Tech grad students – Yunfeng Chen and Lining Arnold Ju – are co-lead authors of the new paper, though they are now on opposite corners of the world. Chen is now doing his work at the Scripps Research Institute in La Jolla, California, and Ju is a researcher with the Heart Research Institute and The University of Sydney in Australia, working in the lab of Shaun Jackson, co-corresponding author with Zhu.
Other researchers on this multi-disciplinary project were: Fangyuan Zhou and, Jiexi Liao (graduate student researchers in the Zhu lab at Georgia Tech); Lingzhou Xues (Penn State University); Qian Peter Su and Dayong Jin (University of Technology Sydney, Australia); Yuping Yuan (Jackson lab at University of Sydney); and Hang Lu (Petit Institute researcher, and professor in the School of Chemical & Biomolecular Engineering at Georgia Tech).
The team used the dual biomembrane force probe technology developed in Zhu’s lab and also fluorescence biomembrane force probe, combined with microfluidic perfusion assays, and applied precisely-controlled mechanical simulations to platelets, identifying an intermediate state of integrin αIIbβ3, whose characteristics are all intermediate between the well-known inactive and active states.
The work reveals distinct integrin state transitions in response to biomechanical and biochemical stimuli, identifying a role for the αIIbβ3 intermediate state in promoting biomechanical platelet aggregation. Using a microfluidic channel that mimics blood vessel stenosis, the researchers could actually see thrombus formation as it happened.
“One of the things we were curious about is, will the mechanical activation of integrins change pathological situations in people with vascular diseases,” says Chen.
The researchers believe that their finding – that biomechanical thrombus growth is mainly mediated by an intermediate state triggered by a biomechanical activation pathway – will probably guide the development of new anti-thrombotic strategies.
This research was supported by grants from the National Institutes of Health (and under its umbrella, the National Institute on Drug Abuse), the National Science Foundation, the Australian Research Council, the University of Technology Sydney, the Diabetes Australia Research Program, the University of Sydney, the Royal College of Pathologists of Australasia, e, the National Science Foundation, and the Cardiac Society of Australia and New Zealand.Release Date: Monday, March 25, 2019
